What is Bacterial Vaginosis?
Bacterial vaginosis (BV) is a common vaginal condition that arises from an imbalance in the natural bacteria present in the vagina. Typically, the vagina maintains a delicate equilibrium of good and bad bacteria; however, when the balance shifts, this condition may ensue. BV is characterized by a predominance of certain types of bacteria, notably Gardnerella vaginalis, leading to symptoms that can be both uncomfortable and concerning for affected individuals.
This condition is prevalent among women, especially those between the ages of 15 and 44. It is significant to note that bacterial vaginosis is not considered a sexually transmitted infection, yet it is more frequently found in women who are sexually active. It is also essential to differentiate BV from other types of vaginal infections, such as yeast infections and sexually transmitted infections (STIs). Unlike yeast infections, which are caused by an overgrowth of Candida species, or STIs like chlamydia and gonorrhea, BV is primarily a result of a microbial imbalance rather than an infection introduced through sexual contact.
Symptoms of bacterial vaginosis can vary, with many women experiencing a thin, grayish-white discharge and a fishy odor, particularly after intercourse. Some women with BV may have no symptoms at all, which can lead to an underdiagnosis of the condition. Recognizing and diagnosing BV is crucial because it can lead to other health complications, including an increased risk of STIs and complications during pregnancy.
Common Symptoms of Bacterial Vaginosis
Bacterial vaginosis (BV) is a prevalent vaginal condition characterized by an imbalance in the normal bacterial flora. One of the most noticeable symptoms is an unusual vaginal discharge. Women may observe a thin, gray or white discharge that often has a different consistency than their usual secretions. This discharge can vary in quantity and may be more pronounced after sexual intercourse or menstruation.
Another significant indicator of bacterial vaginosis is the presence of a strong fishy odor. This characteristic smell is typically more noticeable after sexual activity and can be bothersome for those affected. The odor arises due to the increase of specific bacteria that proliferate in the vaginal environment when BV occurs. It is essential to differentiate this odor from those associated with other vaginal infections, as it is distinctively linked to BV.
In addition to discharge and odor, some women may experience itching or irritation in the vaginal area. This discomfort can lead to feelings of self-consciousness and can affect a woman’s quality of life. However, it is noteworthy that not every woman with bacterial vaginosis will exhibit these symptoms. Many individuals experience minimal to no symptoms and may remain unaware of their condition. This asymptomatic nature can result in underdiagnosis and might lead to complications if appropriate treatment is not pursued.
Overall, being aware of the common symptoms of bacterial vaginosis, including unusual vaginal discharge, fishy odor, and potential discomfort, is crucial for early detection and management. Early recognition can facilitate timely intervention and reduce the risk of further complications associated with this condition.
Causes and Risk Factors
Bacterial vaginosis (BV) is a condition characterized by an imbalance in the naturally occurring bacteria in the vagina. The healthy vagina typically maintains a delicate equilibrium predominantly comprised of Lactobacillus species. Several factors contribute to the disruption of this balance, leading to an overgrowth of harmful bacteria that can cause BV.
One primary cause of bacterial vaginosis is a change in the vaginal pH level. The vagina is usually acidic, which helps to create an environment that supports beneficial bacteria while inhibiting the growth of pathogens. Various circumstances can alter this pH balance, including sexual activity. Engaging in sexual intercourse, particularly with new partners or multiple partners, can introduce various microbes that disrupt the vaginal flora, making the individual more susceptible to BV.
Another significant risk factor is douching, which refers to the process of rinsing the vaginal area with water or chemical solutions. This practice can inadvertently wash away the beneficial bacteria and create an environment that is conducive to the overgrowth of harmful bacteria. Medical professionals discourage douching as a method for vaginal hygiene, as it has been linked to an increased risk of bacterial vaginosis and other vaginal infections.
Certain contraceptive methods may also play a role in the development of bacterial vaginosis. For instance, the use of intrauterine devices (IUDs) has been associated with a heightened risk of BV. Additionally, hormonal changes due to contraceptive pills or other hormonal treatments may impact the natural balance of bacteria in the vagina.
Overall, understanding the causes and risk factors associated with bacterial vaginosis is vital for prevention and management of the condition. By being aware of these influences, individuals can take proactive measures to maintain vaginal health and reduce the likelihood of developing bacterial vaginosis.
Diagnosing Bacterial Vaginosis
Diagnosing bacterial vaginosis (BV) is a multi-faceted process that involves careful evaluation by a healthcare professional. The first step typically entails a comprehensive physical examination, during which the clinician assesses the patient’s symptoms and medical history. It is crucial for individuals experiencing unusual vaginal symptoms, such as an increase in discharge, a fishy odor, or irritation, to discuss these openly with their healthcare provider. Clear communication plays a significant role in guiding the diagnostic process.
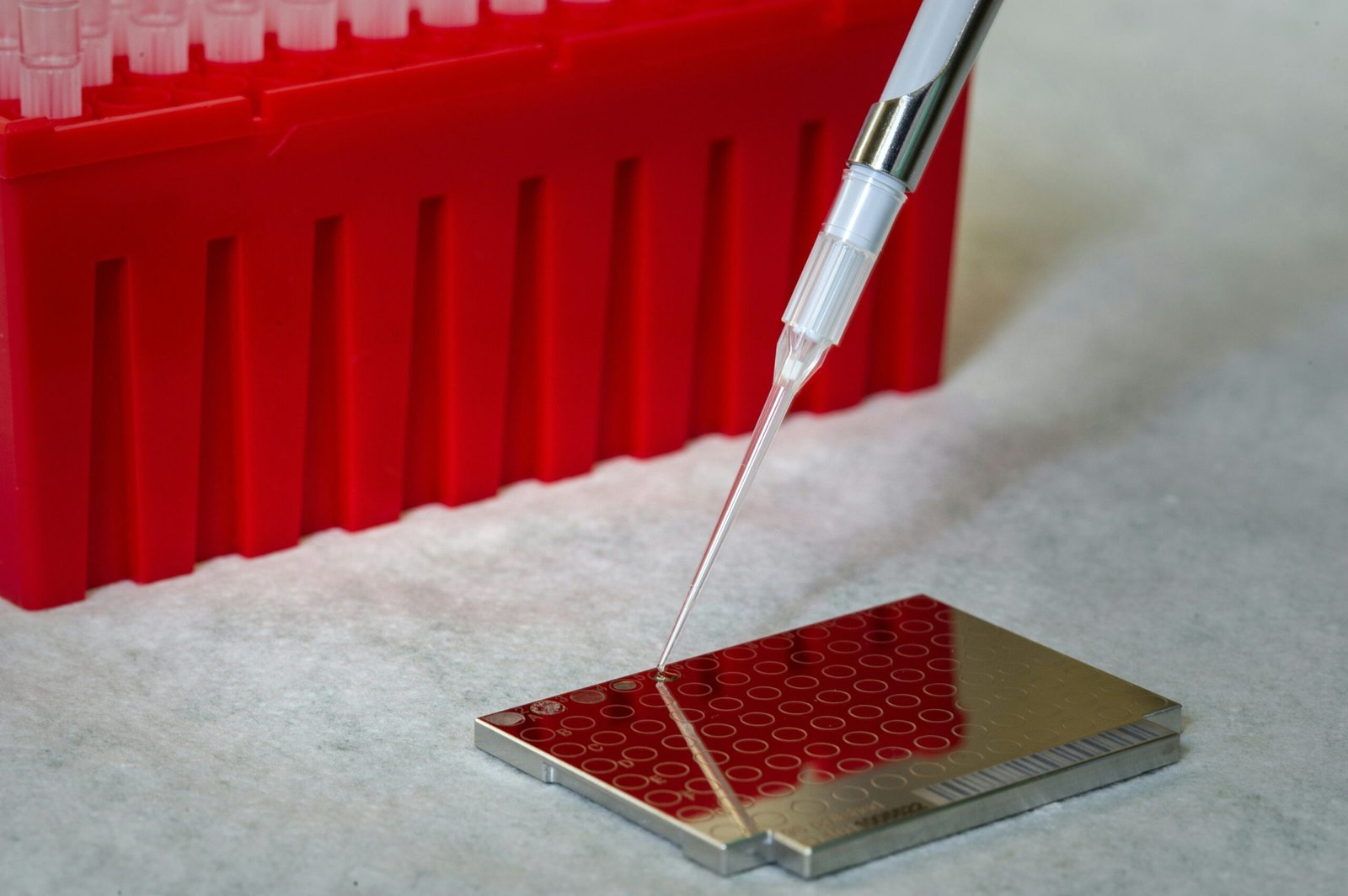
During the physical examination, the healthcare professional may perform a pelvic exam to observe any abnormalities. This examination often includes an analysis of vaginal discharge, which can provide valuable insight into a potential diagnosis. A sample of this discharge may be collected for further laboratory analysis. The characteristics of the discharge, including its consistency and color, can help distinguish bacterial vaginosis from other conditions such as yeast infections or sexually transmitted infections.
In addition to the pelvic examination, laboratory tests are integral to diagnosing bacterial vaginosis accurately. One common method is the pH test, which measures the acidity of the vaginal environment. A pH level greater than 4.5 typically suggests the presence of BV. Another diagnostic tool is the whiff test, where the healthcare provider adds potassium hydroxide to the discharge sample to check for a distinct fishy odor, which is characteristic of BV. These tests are essential in confirming the diagnosis and differentiating BV from other possible infections.
Seeking medical advice is paramount for anyone suspecting they may have bacterial vaginosis. Relying solely on self-diagnosis can lead to incorrect conclusions and inappropriate treatment. A healthcare professional is best equipped to conduct a thorough evaluation and provide an accurate diagnosis, ensuring appropriate treatment and management of symptoms.
Treatment Options for Bacterial Vaginosis
The management of bacterial vaginosis (BV) primarily relies on antibiotic therapy, which may be administered orally or topically. The most commonly prescribed antibiotics for this condition include metronidazole and clindamycin. Metronidazole can be provided in either pill form or as a topical gel, while clindamycin is typically offered as a cream. It is essential for patients to adhere to the prescribed dosage and complete the full course of treatment, even if symptoms improve before finishing the medication. Proper adherence helps to ensure that the infection is entirely eradicated and reduces the risk of recurrence.
Recurrence of BV is a significant concern, with some studies indicating that up to 30% of women may experience a return of symptoms within three months post-treatment. Contributing factors to this recurrence can include both biological and lifestyle elements. Women are encouraged to engage in preventive measures, such as avoiding douching and using scented soaps in the genital area, as these practices can disrupt the natural vaginal flora. It is also advisable to practice safe sex, including the use of condoms, which may help reduce the risk of BV as well as sexually transmitted infections.
Lifestyle changes can also play a critical role in the overall management of bacterial vaginosis. Maintaining good hygiene and establishing a balanced diet rich in probiotics, such as yogurt or fermented foods, may aid in restoring healthy vaginal flora. Some individuals find that limiting their intake of sugar and alcohol can reduce their risk of recurrent infections. It is also beneficial to consult healthcare professionals for tailored advice based on personal health histories and risk factors.
Overall, while effective treatments are available for bacterial vaginosis, ongoing vigilance and proactive lifestyle choices are vital in reducing the likelihood of recurrence and promoting long-term vaginal health.
Preventing Bacterial Vaginosis
Preventing bacterial vaginosis (BV) is an essential part of maintaining women’s reproductive health. By implementing specific strategies, individuals can significantly reduce the risk of developing this condition. A pivotal aspect is the maintenance of a healthy vaginal flora. The vagina hosts a complex ecosystem of bacteria, and maintaining a balance between beneficial and harmful microorganisms is crucial. This can be supported through practices such as wearing breathable cotton underwear and avoiding tight-fitting clothes that may create a humid environment conducive to bacterial overgrowth.
Another critical point is the avoidance of douching and other irritants. Douching can disrupt the natural balance of bacteria, leading to an increased vulnerability to bacterial vaginosis. It is recommended that women refrain from using feminine hygiene products that contain fragrances or harsh chemicals, which can also irritate the vaginal area. Instead, gentle cleansing with water is often sufficient.
Additionally, practicing safe sex is vital in the prevention of BV. Using condoms can help reduce the risk of introducing foreign bacteria into the vagina, which could upset the delicate balance of the microflora. Having a mutually monogamous relationship also lowers the chances of encountering new bacterial strains that could contribute to an imbalance.
Research has highlighted the potential benefits of probiotics as a preventive measure. Probiotics may help restore the natural flora of the vagina, possibly reducing the recurrence of BV. Incorporating probiotic-rich foods such as yogurt, kefir, or fermented vegetables into the diet can be beneficial. Furthermore, maintaining a balanced diet, rich in vitamins and minerals, is recommended to support overall immune function and help regulate the body’s bacterial balance. By being proactive and adopting these preventive strategies, individuals may enhance their chances of avoiding bacterial vaginosis and promoting long-term vaginal health.
Bacterial Vaginosis and Sexual Health
Bacterial vaginosis (BV) is not merely a medical condition; it can significantly impact sexual health and relationships. Women experiencing BV may face various challenges that could affect their sexual pleasure and intimacy with partners. The condition is characterized by an imbalance of the natural bacteria in the vagina, leading to symptoms such as unusual discharge, odor, and irritation. These symptoms may lead to discomfort during sexual activities and can create anxiety regarding sexual encounters, thereby influencing a woman’s confidence and sexual well-being.
The stigma surrounding bacterial vaginosis often adds to the complexity of managing the condition. Many women may feel embarrassed or isolated due to lack of understanding of BV, which can discourage open dialogue with their partners. This communication is crucial, as discussing BV can help alleviate health-related concerns and misunderstandings that may otherwise arise in intimate relationships. A supportive partner can significantly help in navigating the emotional challenges posed by BV, enhancing both partners’ sexual experiences when handled with care and understanding.
Furthermore, research has shown that bacterial vaginosis could increase the risk of acquiring sexually transmitted infections (STIs). The altered vaginal flora associated with BV may compromise the protective mechanisms of the vagina, making it more susceptible to pathogens. Understanding this connection is vital for women and their partners alike, as it emphasizes the importance of regular gynecological check-ups and practicing safe sex to safeguard sexual health. By fostering open communication and support, couples can navigate the complexities of BV together, minimizing its impact on their sexual relationship.
When to See a Doctor
Understanding when to seek medical help for bacterial vaginosis (BV) is essential for maintaining reproductive health. Women experiencing symptoms such as unusual vaginal discharge, a fishy odor, itching, or burning sensations should consider consulting a healthcare provider. While these symptoms may not always indicate bacterial vaginosis, persistent signs that do not improve after a few days warrant professional evaluation.
It is particularly crucial to seek medical consultation if symptoms recur frequently. Recurrent bacterial vaginosis can impact quality of life, signaling the need for a comprehensive medical assessment. This persistence may indicate underlying factors that require treatment, such as hormonal imbalances or lifestyle choices that promote bacterial overgrowth. A healthcare provider can recommend effective treatment options tailored to individual cases, including potential lifestyle adjustments or alternative therapies.
Additionally, it is advisable to consult a doctor if symptoms are accompanied by other concerning issues, such as pelvic pain or symptoms of a urinary tract infection. These signals may suggest complications that extend beyond bacterial vaginosis, necessitating further examination to rule out other diseases. Early detection and professional guidance can prevent complications that could arise if the underlying cause remains untreated.
Women who are pregnant or planning to conceive should also be vigilant. Bacterial vaginosis during pregnancy has been associated with preterm labor and other complications, making it essential to address any symptoms promptly. Seeking timely medical intervention can significantly improve outcomes and ensure both maternal and fetal health.
In summary, recognizing when to seek help for bacterial vaginosis can lead to effective treatment and improved health. Prompt consultation with a healthcare provider can help identify underlying issues and facilitate the management of symptoms, ensuring optimal reproductive health.
Conclusion: Key Takeaways on Bacterial Vaginosis
Bacterial vaginosis (BV) is a prevalent condition that, despite its commonness, often goes unrecognized. Understanding the fundamentals of this vaginal health issue is crucial for women of all ages. BV arises from an imbalance in the natural bacteria typically found in the vagina. The shift in bacterial populations can lead to various symptoms and complications if left untreated. Recognizing the symptoms, which may include unusual vaginal discharge, odor, and discomfort, is the first step toward effective management.
Seeking timely treatment for BV is essential. While the condition is not classified as a sexually transmitted infection, it can still have implications for reproductive health. A healthcare professional can provide a proper diagnosis and treatment plan, which may include antibiotics to restore a healthy bacterial balance. It is imperative for individuals experiencing symptoms or discomfort to consult with a medical provider, as self-diagnosis can lead to worsened conditions or unnecessary anxiety.
Preventative measures contribute significantly to maintaining vaginal health and can reduce the risk of BV recurrence. Some recommended practices include observing proper hygiene, avoiding douching and irritants, and being cautious during sexual activity. Furthermore, maintaining a healthy lifestyle and balanced diet can support overall reproductive health, promoting a stable vaginal microbiome. Regular health check-ups can also aid in early detection and management of BV. In conclusion, comprehending the ins and outs of bacterial vaginosis emphasizes the importance of awareness, timely intervention, and proactive healthcare strategies in safeguarding women’s health.