What is Crohn’s Disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD) that primarily affects the gastrointestinal tract, leading to chronic inflammation which can manifest in various forms and locations. Characterized by periods of remission and flare-ups, Crohn’s can impact the entire digestive tract from the mouth to the anus, although it most commonly affects the end of the small intestine (ileum) and the beginning of the large intestine (colon). This condition is distinguished from another IBD known as ulcerative colitis, which is limited to the colon.
The pathophysiology of Crohn’s disease involves an abnormal immune response that triggers inflammation, ultimately resulting in symptoms such as abdominal pain, severe diarrhea, weight loss, fatigue, and malnutrition. The inflammation in Crohn’s can penetrate deep into the layers of the bowel wall, causing complications like strictures, fistulas, and abscesses. These complications necessitate a comprehensive approach to treatment and management of the disease.
Crohn’s disease can manifest at any age, although it is most commonly diagnosed in young adults and individuals in their late teens to early twenties. The prevalence of Crohn’s disease varies by geographical location, with higher rates reported in developed countries and among individuals of Jewish descent. Recent studies indicate an increasing incidence of Crohn’s disease globally, suggesting that environmental factors, diet, and possibly genetic predisposition may play essential roles in its development. For individuals diagnosed with this condition, understanding the complexities surrounding Crohn’s disease can greatly assist in managing their health and improving their quality of life.
Symptoms of Crohn’s Disease
Crohn’s disease is a chronic inflammatory bowel disease that can present with a variety of symptoms, which may vary significantly from one individual to another. Among the most common symptoms experienced by those affected are abdominal pain and cramping. These discomforts typically occur in the lower abdomen and can be associated with periods of flare-ups, where the inflammation is exacerbated.
Diarrhea is another prevalent symptom of Crohn’s disease, often occurring multiple times a day. This may range from moderately disturbing to debilitating, particularly when paired with urgency, which can significantly affect a person’s quality of life. In some cases, diarrhea may become chronic, contributing to further complications such as dehydration and nutrient malabsorption.
Fatigue is frequently reported by patients suffering from Crohn’s disease. This tiredness is often attributed to the body’s ongoing battle with inflammation and can be exacerbated by inadequate nutrition and sleep disturbances. Furthermore, significant weight loss is another potential symptom. This occurs when the body is unable to absorb essential nutrients or maintain a proper caloric intake due to persistent gastrointestinal distress.
It is crucial to note that symptoms of Crohn’s disease can closely resemble those of other gastrointestinal disorders such as ulcerative colitis or irritable bowel syndrome (IBS). This overlap may lead to challenges in accurate diagnosis, necessitating thorough medical evaluations and tests for proper differentiation. Understanding the symptoms can help in seeking timely medical intervention, as early diagnosis and treatment are essential for managing the condition effectively and improving the patient’s overall wellbeing.
Causes and Risk Factors
Crohn’s disease is a complex and multifactorial condition, with various potential causes contributing to its onset. Research suggests that genetic predispositions play a significant role in determining susceptibility to Crohn’s disease. Individuals with a family history of inflammatory bowel diseases are at a higher risk, indicating that hereditary factors may be influential. Specific genetic mutations have been identified that increase the likelihood of developing the disease, highlighting the importance of genetic screening for at-risk individuals.
Environmental triggers are another critical aspect of Crohn’s disease etiology. Factors such as diet, smoking, and exposure to certain infections may exacerbate or initiate the disease. Studies indicate that a diet high in processed foods and sugar could contribute to inflammation in the gut, potentially leading to the development of Crohn’s disease. Furthermore, smoking has consistently been identified as a significant risk factor; smokers are more likely to develop Crohn’s disease than non-smokers, and the disease often presents with more severe complications in this population.
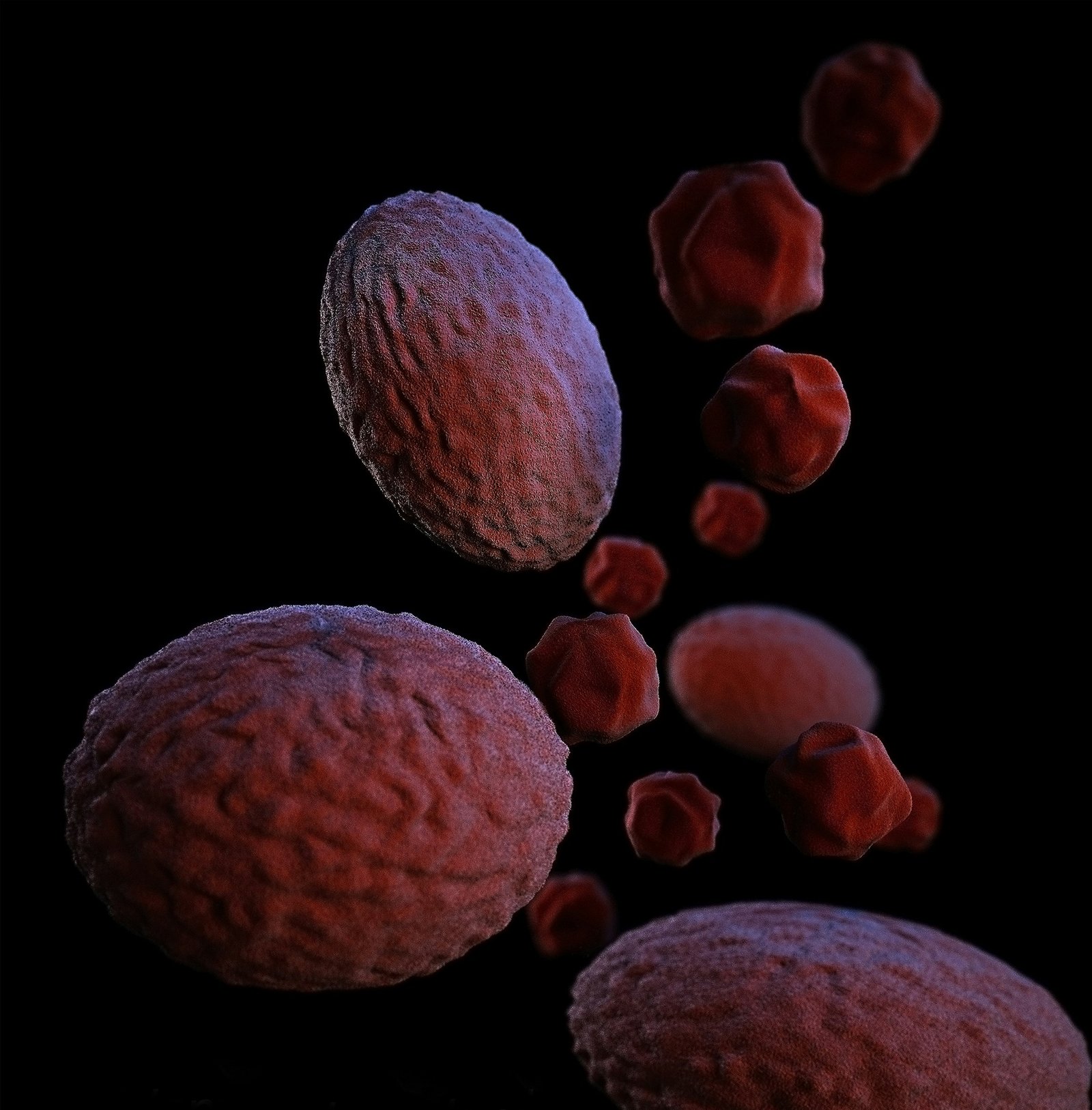
The immune system’s response to gut microflora is another area of investigation in understanding the causes of Crohn’s disease. An abnormal immune response may lead to chronic inflammation, damaging the intestinal lining and triggering the symptoms associated with Crohn’s disease. This abnormality could be influenced by a combination of genetic predisposition and environmental factors, resulting in a dysfunctional immune response in susceptible individuals.
Age is an important risk factor, as Crohn’s disease commonly develops in late adolescence or early adulthood but can be diagnosed at any age. Ethnicity also plays a role, with individuals of Ashkenazi Jewish descent having a higher incidence of the disease compared to other ethnic groups. In summary, the causes and risk factors of Crohn’s disease are multifaceted, involving genetic, environmental, and immunological components that collectively contribute to the disease’s development.
Diagnosis of Crohn’s Disease
Diagnosing Crohn’s disease can be a complex process, as it often shares symptoms with other gastrointestinal disorders. A thorough evaluation by healthcare professionals is essential to accurately identify the condition. The diagnostic process typically begins with a detailed medical history and a physical examination. During this initial assessment, doctors inquire about symptoms, including abdominal pain, diarrhea, weight loss, and fatigue, which are common in individuals with Crohn’s disease.
Following the medical evaluation, several tests may be recommended to confirm the diagnosis. Blood tests are often the first step, as they can provide valuable information about inflammation levels in the body and help assess whether an infection is present. Elevated inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), may indicate an inflammatory condition, prompting further investigation.
Stool tests are another important component of the diagnostic process. These tests are used to rule out infections or blood in the stool, which can mimic symptoms of Crohn’s disease. In cases where stool tests suggest inflammatory bowel disease, imaging studies are usually employed. Techniques such as magnetic resonance imaging (MRI), computed tomography (CT) scans, or ultrasounds allow healthcare providers to visualize the gastrointestinal tract and identify areas of inflammation or lesions indicative of Crohn’s disease.
Endoscopic procedures, including colonoscopy or esophagogastroduodenoscopy (EGD), may also be utilized. These procedures enable direct visualization of the intestinal lining and facilitate biopsy collection to confirm inflammation or other abnormalities. Ultimately, the combination of these diagnostic methods ensures a comprehensive evaluation, allowing healthcare professionals to provide an accurate diagnosis and develop an effective treatment plan for managing Crohn’s disease.
Treatment Options
Crohn’s disease is a chronic inflammatory bowel disease that can significantly impact a person’s quality of life. There is no one-size-fits-all approach to treating Crohn’s disease, and effective management often requires a combination of treatments tailored to the individual’s symptoms and disease severity. The primary treatment modalities include medications, lifestyle modifications, and, in certain cases, surgery.
Medications play a crucial role in managing Crohn’s disease. Anti-inflammatory drugs, such as corticosteroids, are often prescribed to reduce inflammation in the intestines. They can help alleviate flare-ups but are typically used for short periods due to potential side effects. Immune system suppressors, including azathioprine and methotrexate, work by inhibiting the immune response, thereby reducing inflammation and preventing further damage to the intestinal lining. Biologic therapies, which are newer medications, target specific molecules involved in the inflammatory process. These treatments, including infliximab and adalimumab, have shown significant efficacy in managing moderate to severe Crohn’s disease.
In addition to medications, lifestyle changes are vital in managing Crohn’s disease. A well-balanced diet that avoids known triggers can help reduce symptoms. Regular exercise, stress management techniques, and sufficient sleep can also contribute to overall health and wellness. Patients should work closely with healthcare providers, including dietitians, to develop a personalized treatment plan that addresses their specific needs and concerns.
In more severe cases where medications and lifestyle changes do not yield satisfactory results, surgical intervention may become necessary. Surgical options often entail removing the affected portions of the intestine. While surgery can provide lasting relief, it is typically seen as a last resort. The best outcomes occur when treatment plans are individualized, allowing patients to live as symptom-free as possible.
Living with Crohn’s Disease
Managing Crohn’s disease in daily life requires a multifaceted approach that accounts for both physical and emotional well-being. One of the foundational strategies involves dietary management. Patients often benefit from an individualized diet plan that identifies foods that trigger symptoms. Keeping a food diary can assist in recognizing patterns, allowing individuals to avoid problematic items. Many find relief by focusing on a high-protein, low-fiber diet, which can ease digestion during flare-ups while providing necessary nutrients.
Stress management also plays a crucial role in living with Crohn’s disease. Emotional stress is known to exacerbate symptoms for many patients. Techniques such as mindfulness, meditation, and yoga have shown significant promise in reducing stress levels and promoting overall mental health. Regular physical activity, tailored to one’s capabilities, can further enhance mood and physical health, contributing positively to symptom management.
Coping with the emotional toll of Crohn’s disease is another important aspect of daily living. Conversations with healthcare providers about mental health are essential; they can provide resources or referrals to mental health professionals specializing in chronic illness. Peer support groups and counseling can also foster a sense of community and understanding, helping individuals to navigate the challenges associated with the disease.
Encouragingly, maintaining a positive outlook can significantly influence one’s quality of life. Engaging in hobbies, fostering relationships, and setting realistic goals can inspire motivation and hope. Furthermore, building a solid support system consisting of family, friends, and support groups is vital. These connections not only provide emotional support but also practical assistance during difficult times, granting patients the strength to manage their condition successfully.
Complications Associated with Crohn’s Disease
Crohn’s disease, a type of inflammatory bowel disease (IBD), can lead to several complications that significantly impact the patient’s health and quality of life. Understanding these potential complications is crucial for patients and healthcare providers alike, as they influence treatment and management strategies.
One of the most common complications is bowel obstruction, which occurs when the intestine becomes narrowed due to inflammation or scar tissue. This obstruction can lead to severe abdominal pain, vomiting, and distension. In some cases, surgical intervention may be necessary to remove the obstructed portion of the intestine. Management of Crohn’s disease often involves monitoring for symptoms of bowel obstructions, and patients may require adjustments to their treatment plans to minimize inflammation.
Another serious complication associated with Crohn’s disease is the formation of fistulas, which are abnormal connections between different parts of the intestines or between the intestines and other organs such as the bladder or skin. Fistulas can result in infections, malnutrition, and further complications if left untreated. The presence of fistulas often indicates more severe disease and may require aggressive medical management or surgical intervention.
Moreover, individuals diagnosed with Crohn’s disease have an increased risk of developing colorectal cancer. Chronic inflammation over time can lead to dysplasia, a precancerous change in the cells lining the colon. Regular surveillance colonoscopies are recommended for patients, particularly those who have had Crohn’s disease for several years. Early detection is vital, as it allows for timely intervention and better management of any potential malignant transformations.
In conclusion, complications such as bowel obstructions, fistulas, and an elevated risk of colorectal cancer necessitate a comprehensive approach to treatment and management of Crohn’s disease. By staying vigilant and regularly consulting healthcare providers, patients can better navigate the complexities of their condition and prevent the severity of these complications.
Research and Advances in Crohn’s Disease Treatment
The landscape of Crohn’s disease treatment has significantly evolved over the past few years, driven by rigorous research and the pursuit of innovative therapeutic approaches. Currently, researchers are exploring a multitude of potential therapies aimed at addressing the underlying inflammation and symptoms of Crohn’s disease. One promising area of focus is the development of biologic drugs, which target specific pathways in the immune response that contribute to inflammation. These medications, such as anti-TNF agents, have shown great success in reducing the frequency and severity of flare-ups among patients with moderate to severe forms of the disease.
In addition to biologics, there is considerable interest in novel small molecules which can inhibit inflammatory pathways that play a critical role in Crohn’s disease. For instance, medications like JAK inhibitors have emerged as a new class of treatments that may offer patients enhanced options compared to traditional therapies. Researchers are also investigating the potential of stem cell therapy as a means to regenerate the intestinal lining, potentially providing relief and promoting healing in patients afflicted with Crohn’s disease.
Clinical trials are essential in assessing the efficacy and safety of these emerging therapies. Numerous trials are underway, specifically targeting the mechanistic understanding of Crohn’s disease and incorporating patient-specific factors into treatment plans. These initiatives aim not only to provide relief but also to find a long-term solution for better management of the disease. As we look towards the future, the direction of Crohn’s disease management appears increasingly personalized, leveraging advancements in genomics and biomarker discovery to tailor treatments according to individual patient profiles.
Continued research and patient participation in clinical trials are vital in uncovering new strategies and therapies that could redefine standard treatment practices for Crohn’s disease, fostering a greater understanding of the condition and ultimately improving patient outcomes.
Resources and Support for Crohn’s Disease Patients
For individuals living with Crohn’s disease, access to resources and support is vital for managing the condition and improving quality of life. Various organizations and platforms provide significant assistance to patients and their families, ensuring they receive the necessary information, advocacy, and community support.
One prominent resource is the Crohn’s & Colitis Foundation, which offers extensive educational materials, support groups, and advocacy initiatives. This foundation not only aids in fostering connections among patients but also aims to increase awareness and research funding for inflammatory bowel diseases (IBD) such as Crohn’s disease. Their extensive network of local chapters facilitates community engagement, allowing patients to share their experiences and find emotional support among peers who understand their challenges.
In addition to national organizations, many online platforms have emerged to provide valuable information and forums for discussion. Websites like Healthline and WebMD feature comprehensive guides on Crohn’s disease, including treatment options, dietary guidelines, and lifestyle tips. Social media platforms also serve as informal support networks, where individuals can connect with others facing similar circumstances, share stories, and seek advice in real time.
Patient advocacy groups play a significant role in offering resources tailored to specific needs of Crohn’s patients. For example, the American Gastroenterological Association provides access to information on clinical trials and research updates, connecting patients with cutting-edge treatments. Furthermore, many hospitals and clinics host support groups led by healthcare professionals, ensuring patients can express their feelings and discuss coping strategies in a safe environment.
The journey through Crohn’s disease can be daunting, but the availability of resources and support networks is essential. Establishing connections within these communities can lead to improved emotional well-being and a better understanding of the disease, ultimately resulting in a more empowered approach to living with Crohn’s disease.